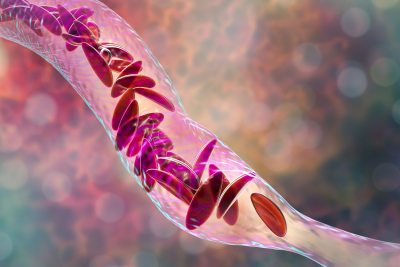
New Brunswick, N.J., September 1, 2023— Sickle cell disease, a genetic disorder that affects red blood cells, causes significant health problems for children, which can worsen as they become adults and even shorten their lifespan. In recent years, bone marrow transplant (BMT), also known as stem cell transplant, has emerged as a potential curative approach for the disease. When a child with sickle cell disease undergoes a BMT, he or she receives healthy bone marrow that produces normal red blood cells. Niketa C. Shah, MD, chief of Pediatric Bone Marrow Transplantation and Cellular Therapies at Rutgers Cancer Institute of New Jersey and associate professor of pediatrics at Rutgers Robert Wood Johnson Medical School, shares more about this process for parents.
What may be the benefits of BMT for a child with sickle cell disease?
A blood or marrow transplant (BMT) stands as the sole established cure for Sickle Cell Disease (SCD). Unlike surgery, BMT constitutes a treatment wherein healthy blood-forming cells are extracted from a donor and then delivered to you via an intravenous (IV) infusion. This process aims to substitute the unhealthy sickle cells with healthy ones. While BMT cannot undo organ damage resulting from SCD, it does possess the capability to prevent further damage.
How is eligibility for BMT determined for a child with sickle cell disease?
Transplants have demonstrated notable efficacy, particularly among children with a match sibling donor. In cases where a matched sibling donor is unavailable, numerous patients opt to undergo a transplant through participation in a clinical trial. Initiating a conversation with your doctor regarding the most suitable treatment path for your current situation holds great significance. Transplantation might be advised by medical professionals if you have experienced:
-
Over three instances of severe pain crises within the past two years
-
A stroke or a silent stroke
-
Acute chest syndrome occurring two or more times in the preceding two years
-
Eight or more red blood cell transfusions within a single year
-
Pulmonary hypertension
-
Chronic pain persisted for more than six months
-
Ultrasounds indicate a heightened risk of stroke
What does the BMT process look like for a child?
First, the child will get chemotherapy, and sometimes radiation, to get rid of the problem blood cells. Then, the donor's special blood cells (bone marrow cells) will be put into the child’s body through a thin tube in your vein, like when you get a blood transfusion.
These special cells will go to your bone marrow and help make strong red blood cells, white blood cells, and platelets. The whole process, from treatment to getting better, can take many months or even years.
What type of care will my child need after a transplant?
Once your child's doctors confirm that the transplant was successful, your child can leave the hospital. It could take 6 to 12 months or even longer for your child's blood cells and immune system to return to normal. While this is happening, it's important for your child to take all the medicines the doctor gives for the transplant. This makes sure your child's body doesn't reject the new cells and prevents infections. The doctor will carefully monitor your child's health during this period.
The Pediatric Stem Cell Transplantation and Cellular Therapies Program at Rutgers Cancer Institute, the state’s leading cancer program and only NCI-designated Comprehensive Cancer Center together with RWJBarnabas Health, is one of the only programs in the state of New Jersey that utilizes stem cell transplants in the treatment of benign diseases in children such as sickle cell disease, thalassemia, immune system disorders, bone marrow failure disorders and inherited metabolic disorders.

