Story by Michele Fisher • Portraits by Nick Romanenko View the complete magazine | Subscribe to Cancer Connection
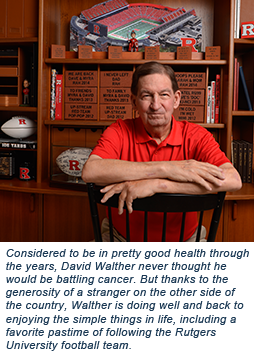
When David Walther was diagnosed with acute myeloid leukemia, he put his trust in the expertise of those in the Blood and Marrow Transplant Program at Rutgers Cancer Institute of New Jersey and its flagship hospital Robert Wood Johnson University Hospital (RWJ). But he had no idea at the time that his recovery would also depend on the generosity of a total stranger on the other side of the country - an ‘angel’ who is now considered ‘part of the family.’
 The ride home from his job as a supervisor in the New Jersey Department of Military and Veterans Affairs in March 2013 was typical at first – until the searing pain in his left arm hit. David Walther wondered, “Am I having a heart attack?” That scare immediately prompted this grandfather of two to go to his local hospital, where they kept him overnight for observation and a bone marrow biopsy – due to low blood counts. Discharged the next morning, Walther resumed his normal activities, assured that his heart was fine. A few days later, however, he received the call that he had acute myeloid leukemia (AML). “They told me to stop what I was doing and immediately get to New Brunswick, where they had arranged for me to meet with Dr. Roger Strair. They gave me instructions as to what to do if I developed a fever or started bleeding on the drive there. I had always been vigilant about my health. I had no symptoms. The news was numbing,” the 70-year-old Walther recalls.
The ride home from his job as a supervisor in the New Jersey Department of Military and Veterans Affairs in March 2013 was typical at first – until the searing pain in his left arm hit. David Walther wondered, “Am I having a heart attack?” That scare immediately prompted this grandfather of two to go to his local hospital, where they kept him overnight for observation and a bone marrow biopsy – due to low blood counts. Discharged the next morning, Walther resumed his normal activities, assured that his heart was fine. A few days later, however, he received the call that he had acute myeloid leukemia (AML). “They told me to stop what I was doing and immediately get to New Brunswick, where they had arranged for me to meet with Dr. Roger Strair. They gave me instructions as to what to do if I developed a fever or started bleeding on the drive there. I had always been vigilant about my health. I had no symptoms. The news was numbing,” the 70-year-old Walther recalls.
Roger Strair, MD, PhD, leads the Blood and Marrow Transplant Program at Rutgers Cancer Institute, where he collaborates with a team of experts focused on cancers of the blood – including hematologist/oncologist, Vimal Patel, MD, who was brought in on the case. Both physicians are faculty members at Rutgers Robert Wood Johnson Medical School.
AML is a cancer of the blood and bone marrow. The “acute” in AML refers to the fast progression of the disease. It is a “myeloid leukemia” because it affects a group of white blood cells called myeloid cells that normally develop into various types of mature white blood cells, red blood cells and platelets. AML develops due to genetic changes in a precursor cell of myeloid lineage. These changes alter normal growth and differentiation of these cells, resulting in an accumulation of large numbers of abnormal, immature myeloid cells in the bone marrow and peripheral blood. The consequence is a constellation of signs and symptoms that may mimic the flu such as fevers, bone pain, lethargy, fatigue, shortness of breath, infections, easy bruising and unusual bleeding. The most common type of acute leukemia in adults, AML can progress quickly if not treated.
 Dr. Patel would first put Walther on induction chemotherapy to kill the leukemia cells in the blood and marrow in order to put the cancer in remission. But that’s only the first step. Post-remission therapy is then administered to kill any remaining leukemia cells that could pose a risk for a relapse, but not every patient will respond favorably to the same treatment. “We learned from Dr. Patel that David needed to be in the hospital for the next 31 days,” recalls Walther’s wife Myra. “The gravity of those words was not lost on us.”
Dr. Patel would first put Walther on induction chemotherapy to kill the leukemia cells in the blood and marrow in order to put the cancer in remission. But that’s only the first step. Post-remission therapy is then administered to kill any remaining leukemia cells that could pose a risk for a relapse, but not every patient will respond favorably to the same treatment. “We learned from Dr. Patel that David needed to be in the hospital for the next 31 days,” recalls Walther’s wife Myra. “The gravity of those words was not lost on us.”
Admitted to RWJ under the care of the Rutgers Cancer Institute team, Walther was started on induction therapy consisting of two standard chemotherapy agents, idarubicin and cytarabine. The aim was to kill off the cancer cells so Walther’s healthy white blood cells could develop. “Early during the induction chemotherapy, we received genetic data from the leukemia cells,” explains Patel. “In Mr. Walther’s case, we found multiple complex chromosomal abnormalities which portends an unfavorable prognosis. It was clear that post-remission chemotherapy alone would not reduce his risk of relapse. What he needed was a bone marrow transplant – the help of someone else’s healthy, leukemia-free stem cells that would replace the unhealthy marrow and produce immune cells capable of fighting the leukemia.
Transplant Coordinator Mary Kate McGrath, MSN, RN, APN-C, OCN, BMTCN, got to work on finding a suitable donor through the National Marrow Donor Program registry – a process that often takes some time. “Given that Mr. Walther is Caucasian, the odds were better for finding the right candidate,” notes Patel, adding that despite 12.5 million selfless volunteers who stand ready to be a bone marrow donor in the Be the Match Registry, not all populations are as fortunate in finding a match (see sidebar). While the process of locating a matched donor continued, Walther received an additional two cycles of chemotherapy – stretching his 31 days to 92 over the next five months.
Trisha’s Story
Around 1996, Trisha Marchant learned of a child in her Utah neighborhood with an immunodeficiency disease known as Wiskott-Aldrich Syndrome, for which a bone marrow transplant is the only known cure. This neonatal intensive care nurse was inspired to put herself on the national bone marrow registry. Fast forwarding 17 years she learned a friend was diagnosed with AML. It made her think about the registry and wonder if they still had her on the list. Just three weeks later, she received the devastating news that her friend had passed away. “It was on that very day I received a call from the registry saying my tissue was a match for a candidate. It was meant to be,” remembers a tearful Marchant. “My husband and four sons were on board with my decision and” – at 48-years old – “I began the process with some blood tests in May (2013).”
Three Minutes
Blood cancer is an all-inclusive term for malignancies of the blood, bone marrow or lymph nodes that affect normal blood cell production or function. As these malignant blood cells proliferate, they cause life-threatening damage to the hematologic and immune systems. Many patients will need months of intensive chemotherapy and for others, the best chance at survival will be a stem cell transplant. This potentially lifesaving therapy is a form of immune therapy that works with the donor stem cells (from the bone marrow, peripheral blood, or umbilical cord) giving rise to a new immune system having the potential to view the cancerous cells as foreign and leading to their eradication. About 30 percent of patients in the United States will be able to find a matching donor within their families, but 70 percent - nearly 14,000 each year - must rely on the selflessness of a stranger to donate their stem cells. The unrelated-donor registries of adult volunteers and banked umbilical cord-blood units, such as the Be the Match Registry operated by the National Marrow Donor Program (NMDP), provide potential sources of donors. The NMDP has grown to include over 12.5 million volunteers and more than 200,000 cord-blood units. Despite this, six of 10 patients will be unable to find a suitable donor. The probability is even lower for those of diverse ancestry (African Americans, Native Americans, Alaskan natives, Asians including South Asians, Pacific Islanders including Hawaiian natives and Hispanics). This is due to the genetic variability within these ethnic/race groups and the under-representation of these groups in the registries. Clearly there is a need to recruit additional donors into the registries. Key is focusing on recruitment strategies that target donors from these groups with low probabilities of finding a donor. Registering is easy and requires mailing back a swab of cheek cells that are used for tissue typing and matching. On average, one in 500 members will be selected to donate their stem cells – a potentially lifesaving measure. To learn more, visit BeTheMatch.org. ■ (Sources: BeTheMatch.org and Gragert et al, (2014) HLA match likelihoods for hematopoietic stem cell grafts in the U.S. registry, ‘New England Journal of Medicine,’ 371:339-48) |
Donors and patients are matched by their specific human leukocyte antigen (HLA) types, which is very different than matching blood types. The best outcomes happen when a patient’s HLA and the HLA of the donor is a close match. HLA is a protein or marker found on most cells of the body. The immune system uses HLA markers to know which cells belong in the body and which do not. There are more than 13,000 HLA markers which results in an infinite number of combinations for one person. What is critical to a successful transplant however, involves the matching of only certain markers. An ideal match would be a match at a minimum of eight basic HLA markers. A close match is essential for the engraftment of new healthy cells and reduces the risk of a post-transplant complication called graft-versus-host disease (GVHD). Some transplants can move forward with a lower number match, but overall survival may not be as favorable, says Patel. Marchant was an eight out of eight HLA match. It was determined that she would give peripheral blood stem cells – a type of stem cell transplant that is similar to bone marrow or umbilical cord stem cells but different in how the cells are harvested.
The closest collection agency to Marchant’s Utah home was in Berkeley, California. But before the harvesting, which is a non-surgical process also known as apheresis, Marchant underwent a five-day preparation that included injections of a medicine to boost the production of blood stem cells. On the day of the donation, blood was removed through a needle in one of Marchant’s arms and passed through a machine that separated out the stem cells. The remaining blood returned to her via the other arm. “I think people have the misconception that surgery is involved – it’s not. It was really no different than giving blood or platelets, with the exception that it lasted about five hours. My bones felt slightly achy afterwards, but that was it,” she shares, adding the preparation was simple too. One thing she thought was interesting “was that they actually asked me to refrain from skydiving!” “There’s a good reason for that,” interjects Patel. “It’s a leap of faith,” he says, (no pun intended) “because part of the transplant involves a conditioning regimen where we kill the patient’s (diseased) marrow cells with chemotherapy before the donor cells are even harvested. We’re counting on the donor’s stem cells to come in – so if there is an accident that delays or prevents the harvesting of these cells, the outcome is most likely grave.” Marchant recalls being told, “If you back out, the patient will die.”
The Big Day
The Walthers were informed of a matched donor. Keep in mind, there was no face or name to put with this person – just the knowledge that someone out there was generous enough to give of themselves in this way – “an angel,” says Walther. They were grateful. Due to confidentiality policies, donors and recipients are not permitted to have direct contact with each other for at least one year, however each case is unique and waiting periods may even be longer.
On August 6, 2013, a nurse came into Walther’s room with a small ice cooler containing the harvested cells and told him they would soon be ready for the transplant. The cells would be infused into Walther’s body much the same way as they were collected from Marchant. “I thought there would be more to it. When she brought the little cooler in, I thought it might be her lunch!” acknowledges Walther’s wife with a laugh.
But before the infusion took place, the cells were taken into the lab and evaluated to see how many stem cells there were and if they were in good condition. Prior to the infusion, Walther received chemotherapy over the course of a few days - designed to cleanse his bone marrow, suppress his immune system, and kill any remaining leukemia cells so that the body would be less likely to reject the new stem cells. This was followed by the infusion – a 30-minute procedure in which the harvested stem cells are transfused into the recipient. It takes about two weeks for those newly-infused cells to grow and develop into mature blood cells. Some of these immune cells become not only infection fighters but also leukemia fighters in the recipient to reduce the risk of the disease relapsing.
For the most part, Walther responded well, says his doctor. Walther visited with Patel and the team twice a week for the first 100 days. He was placed on immunosuppressive medications designed to calm the donor cells, as “they can be feisty at first,” shares Patel. That first 100 days was a bit challenging, as Walther experienced fatigue, hair loss, and changes to his skin. “We had to keep our home extremely clean to avoid infection and to adhere to dietary restrictions and strict food preparation guidelines,” adds his wife. Six months into his recovery, Walther had his first bout of graft-versus-host disease; however, with the careful monitoring by Patel, his symptoms were well managed. “I would not be where I am today were it not for the love and support of my wife and the excellent care of my doctor.”
A Special Anniversary
 Marchant received a one-month update from the registry letting her know her recipient was doing well. Still – no names were attached. One year post transplant, Walther was still doing well and he and his wife were eager to connect with the donor. Bone marrow transplant coordinator Jackie Manago, RN, BSN, BMTCN, reached out through the registry, gaining Marchant’s information and contacted her. She received a quick response back. “We sent flowers to Trisha,” recalls Walther’s wife. “We wanted that first contact to be meaningful.” E-mails, letters and texting soon followed. Walther then called, leaving a message for Marchant who was not home at the time. “It was hard for him to make the initial call,” says Myra Walther. “It was extremely emotional for him. I listened in. He said ‘I love you’ at the end.” “I played that voicemail over and over,” Marchant fondly remembers.
Marchant received a one-month update from the registry letting her know her recipient was doing well. Still – no names were attached. One year post transplant, Walther was still doing well and he and his wife were eager to connect with the donor. Bone marrow transplant coordinator Jackie Manago, RN, BSN, BMTCN, reached out through the registry, gaining Marchant’s information and contacted her. She received a quick response back. “We sent flowers to Trisha,” recalls Walther’s wife. “We wanted that first contact to be meaningful.” E-mails, letters and texting soon followed. Walther then called, leaving a message for Marchant who was not home at the time. “It was hard for him to make the initial call,” says Myra Walther. “It was extremely emotional for him. I listened in. He said ‘I love you’ at the end.” “I played that voicemail over and over,” Marchant fondly remembers.
Special gifts to one another to “break the ice” were sent – and Marchant hung a photo of the Walthers in her home. “I now have family in New Jersey,” she says. The bond grew even more when Mrs. Walther casually mentioned to Marchant that she was planning a special party in New Jersey in August 2015 to mark the two-year anniversary of the transplant. Marchant asked if she could fly in from Utah to surprise him. “I was overwhelmed at her graciousness and the prospect of having the opportunity to thank her face to face for this precious gift of life,” says Mrs. Walther. So, exactly two years to the day of the transplant, donor and recipient finally embraced at the airport. They spent five days together, learning about each other and the bond that they now share.
Marchant jokes with Walther that he needs to remember he has some of her T-cells now – a type of white blood cell important to the immune system. “‘T’ not only stands for ‘Trisha,’” she muses, “but also for ‘together.’” An unintended pairing, this duo of donor and recipient has expanded the definitions of ‘together’ and ‘family’ – and ‘angel.’ “It’s amazing to me that something so simple saved someone’s life,” notes Marchant. “I would do it again.” ■


