New Brunswick, N.J., December 6, 2020 – Researchers from Rutgers Cancer Institute of New Jersey, the state’s only National Cancer Institute-designated Comprehensive Cancer Center, evaluated the frequency of SARS-CoV-2, the virus that causes COVID-19, on various environmental surfaces in outpatient and inpatient hematology/oncology settings located within Rutgers Cancer Institute and Robert Wood Johnson University Hospital, an RWJBarnabas Health facility. The study revealed extremely low detection of SARS-CoV-2 on environmental surfaces across multiple outpatient and inpatient oncology areas, including an active COVID-19 floor. Andrew M. Evens, DO, MSc, FACP, associate director for clinical services and director of the Lymphoma Program at Rutgers Cancer Institute and medical director of the oncology service line at RWJBarnabas Health, is senior author of the work, which is being presented during the virtual American Society of Hematology Annual Meeting this week.
Evidence suggests that mortality due to COVID-19 is higher in patients with cancer due to frequent visits to healthcare settings. Patients harboring hematologic malignancies, which are cancers that affect the blood, bone marrow, and lymph nodes, have the highest mortality due to the virus. While COVID-19 is transmitted person to person through respiratory droplets, it has been hypothesized that there is a potential risk of SARS-CoV-2 spreading via contact with contaminated surfaces and equipment, especially in healthcare settings, creating additional concern for patients with blood cancers.
“Compared with other cancer patients, those with hematologic cancers have demonstrated a potential higher mortality in conjunction with SARS-CoV-2 infection, so further understanding about COVID-19 transmission in high impact areas where these patients receive their care is needed,” notes Dr. Evens, who is also a professor of medicine at Rutgers Robert Wood Johnson Medical School. “Our findings suggest that contamination by SARS-CoV-2 on surfaces and equipment in hematology/oncology areas is extremely low, demonstrating that enhanced safety policies are effective and patients with blood cancers frequenting these areas should have minimal concerns.”
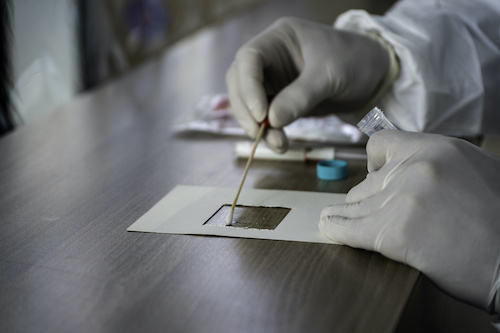
Environmental swabbing took place in two outpatient clinics including the malignant hematology and medical oncology units and infusion suites as well as inpatient areas which included the leukemia/lymphoma/CAR T-cell unit, and an inpatient unit caring for patients actively infected with COVID-19. Surfaces were sampled on Mondays, Wednesdays and Fridays from June 17, 2020 through June 29, 2020. Areas included waiting rooms, infusion areas, bathrooms, floors, elevator banks, doors, and exam rooms, computer equipment, pneumatic tubing stations, pharmacy benches, and medication rooms. Medical equipment was also swabbed from these areas including intravenous poles, chemotherapy bags, vitals monitor, telemetry stations, and linen carts.
Analysis of the 130 samples collected were separated into three categories: patient/public areas (85), staff areas (22), and medical equipment (23). In the two outpatient clinics and inpatient leukemia/lymphoma/CAR T-cell unit, no SARS-CoV-2 was detected on any swabbed surfaces. In the inpatient COVID unit, one patient/public sample was positive for detection of SARS-CoV-2 in an area where a patient with recent infection was receiving treatment. Thus, the overall positive test rate for SARS-CoV-2 across all surfaces in the combined outpatient and inpatient hematology/oncology units was a low 0.5 percent.
The authors note study limitations including the inability to analyze the complete surface area of the varied locations, which may have reduced sensitivity. In addition, researchers did not attempt to culture SARS-CoV-2 from the one positive sample; it is unknown if it contained live virus. Continued studies are needed to monitor rates of virus transmission and the environmental factors involved in the propagation of the SARS-CoV-2 infection.
This work was supported in part by a National Cancer Institute Cancer Center Support Grant (P30CA072720). Additional details including author contributions, exemptions and conflicts of interest can be found here.
About Rutgers Cancer Institute of New Jersey
As New Jersey’s only National Cancer Institute-designated Comprehensive Cancer Center, Rutgers Cancer Institute, together with RWJBarnabas Health, offers the most advanced cancer treatment options including bone marrow transplantation, proton therapy, CAR T-cell therapy and complex surgical procedures. Along with clinical trials and novel therapeutics such as precision medicine and immunotherapy – many of which are not widely available – patients have access to these cutting-edge therapies at Rutgers Cancer Institute of New Jersey in New Brunswick, Rutgers Cancer Institute of New Jersey at University Hospital in Newark, as well as through RWJBarnabas Health facilities. To make a tax-deductible gift to support the Cancer Institute of New Jersey, call 848-932-8013 or visit www.cinj.org/giving.
###
For journalists – contact:
Krista Didzbalis
Media Relations Assistant
908-812-6114
krista.didzbalis@rutgers.edu
For patient appointments/inquiries – contact:
844-CANCERNJ (844-226-2376)

